Antibiotic resistance kills over 1mn people a year, says study

Roula Khalaf, Editor of the FT, selects her favourite stories in this weekly newsletter.
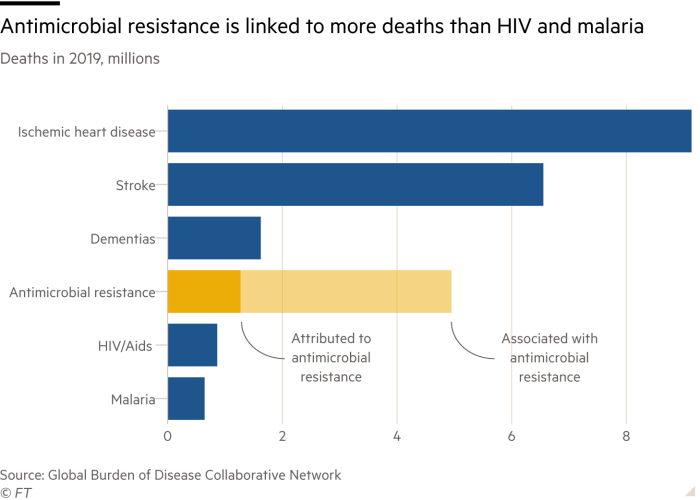
More than 1mn people around the world die each year from infections linked to microbes resistant to antibiotics, according to a study that estimates the scale of a “silent pandemic” that is now more deadly than malaria or HIV.
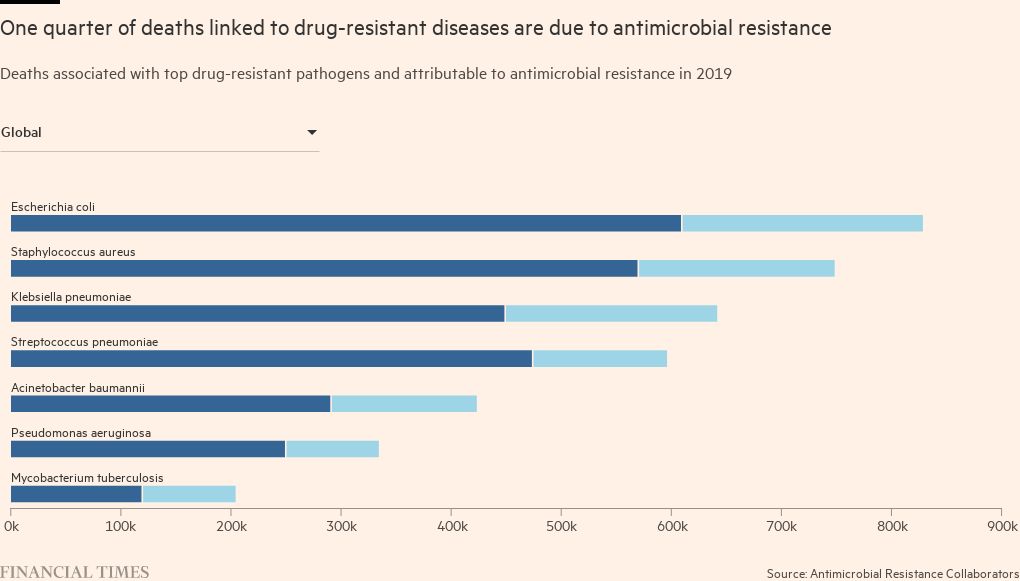
The analysis published in the Lancet medical journal calculates that 1.27mn deaths in 2019 were the direct result of drug resistant bacterial infections and 4.95m deaths were associated with them. That represents a sharp jump from previous estimates of 700,000 deaths a year.
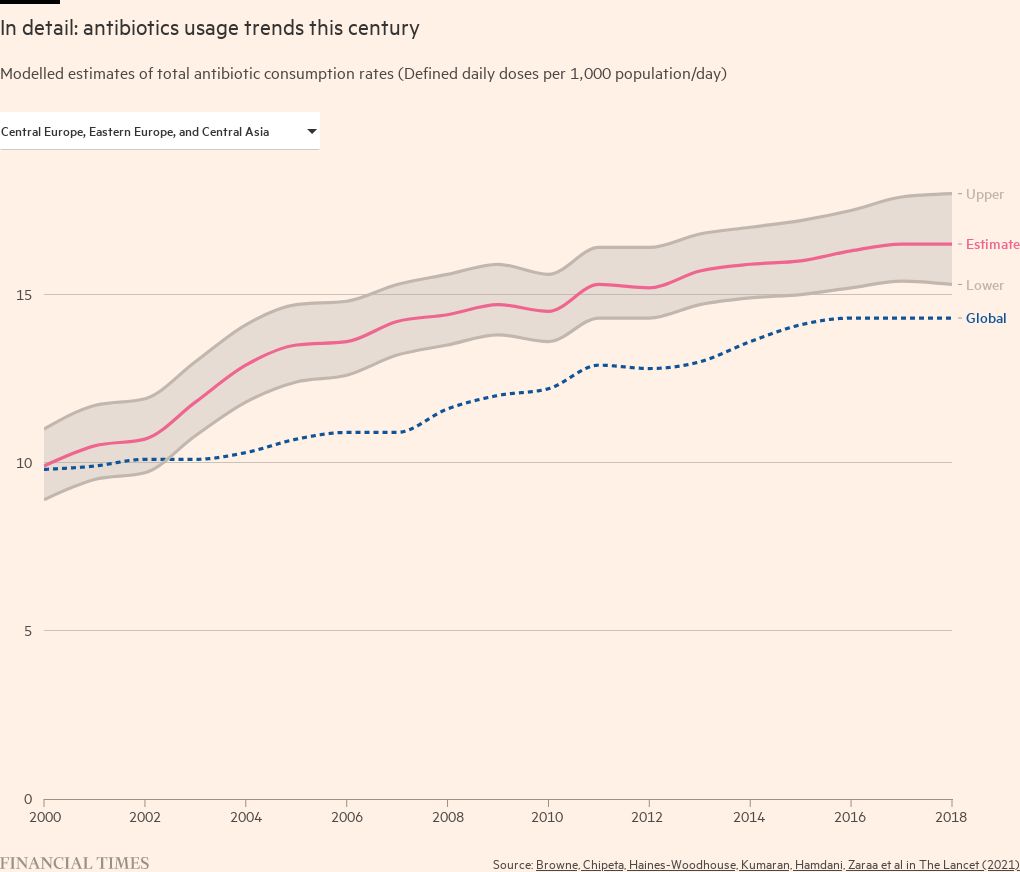
Antimicrobial resistance (AMR) has been described by experts as one of the greatest threats to public health in the 21st century. The figures underscore the dangers of bacteria developing resistance to existing antibiotics as a result of overuse — including during the Covid-19 pandemic — against a backdrop of scant new vaccines and drugs under development to prevent or treat infections.
Hanan Balkhy, assistant director at the World Health Organization, said: “I still think it is an underestimate of the reality. AMR is truly an existential threat to modern medicine in high, mid and low income countries.”
Chris Murray, head of the Institute for Health Metrics and Evaluation at the University of Washington, one of the co-authors, said the issue of what share of the 4.95mn of patients with resistant infections died as a direct result was “hotly contested” but thought it was closer to the figure of 1.27mn cited in the analysis.
The study — funded by the Bill & Melinda Gates Foundation, the Wellcome Trust and the UK’s Department of Health and Social Care — is based on modelling that draws on a broad range of data sources including hospital records, laboratory results and surveillance information from pharmaceutical companies and public health specialists.
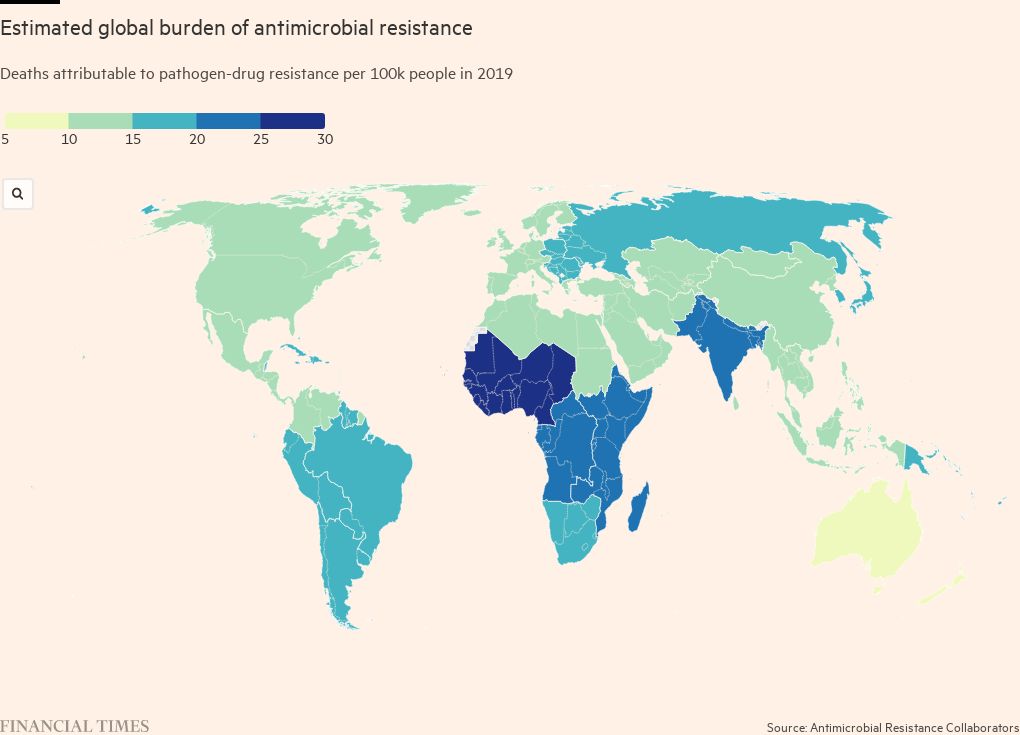
The analysis revealed that the burden of AMR-linked deaths as a share of total mortality varies widely around the world and is highest in western Africa, followed by eastern Africa and south Asia.
While rates of antibiotic use are higher in other regions including the Middle East, the researchers concluded that the deaths reflect the combination of both the extent to which resistant bacteria are circulating and the underlying frequency of critical infections such as lower respiratory, bloodstream and intra-abdominal infections.
They also pointed to limited testing capacity, inappropriate use, inadequate supplies of more expensive and targeted medicines, poor sanitation and the circulation of substandard and counterfeit drugs.
The authors called for enhanced infection prevention and control, increased vaccination including for bacterial pneumonia, reduced use of antibiotics in farming, cutting inappropriate use in humans such as to treat viruses, and fresh investment to develop newer replacement drugs.
Jim O’Neill, a former UK minister who chaired a 2016 review that estimated antimicrobial resistance would cost the global economy $100tn by 2050 without further action, said: “These numbers are much bigger than we assumed. That should result in much more significant concern. They suggest Covid-19 is just a warm up for what could happen if we don’t sort out AMR.”
He called for greater involvement of financial policymakers alongside health specialists around global health threats, improved disease surveillance systems and increased funding including for the WHO.
O’Neill is among a number of experts who last year recommended the creation of a finance and health board by the G20 to help tackle pandemics, but which met resistance from a number of emerging economies.

Comments